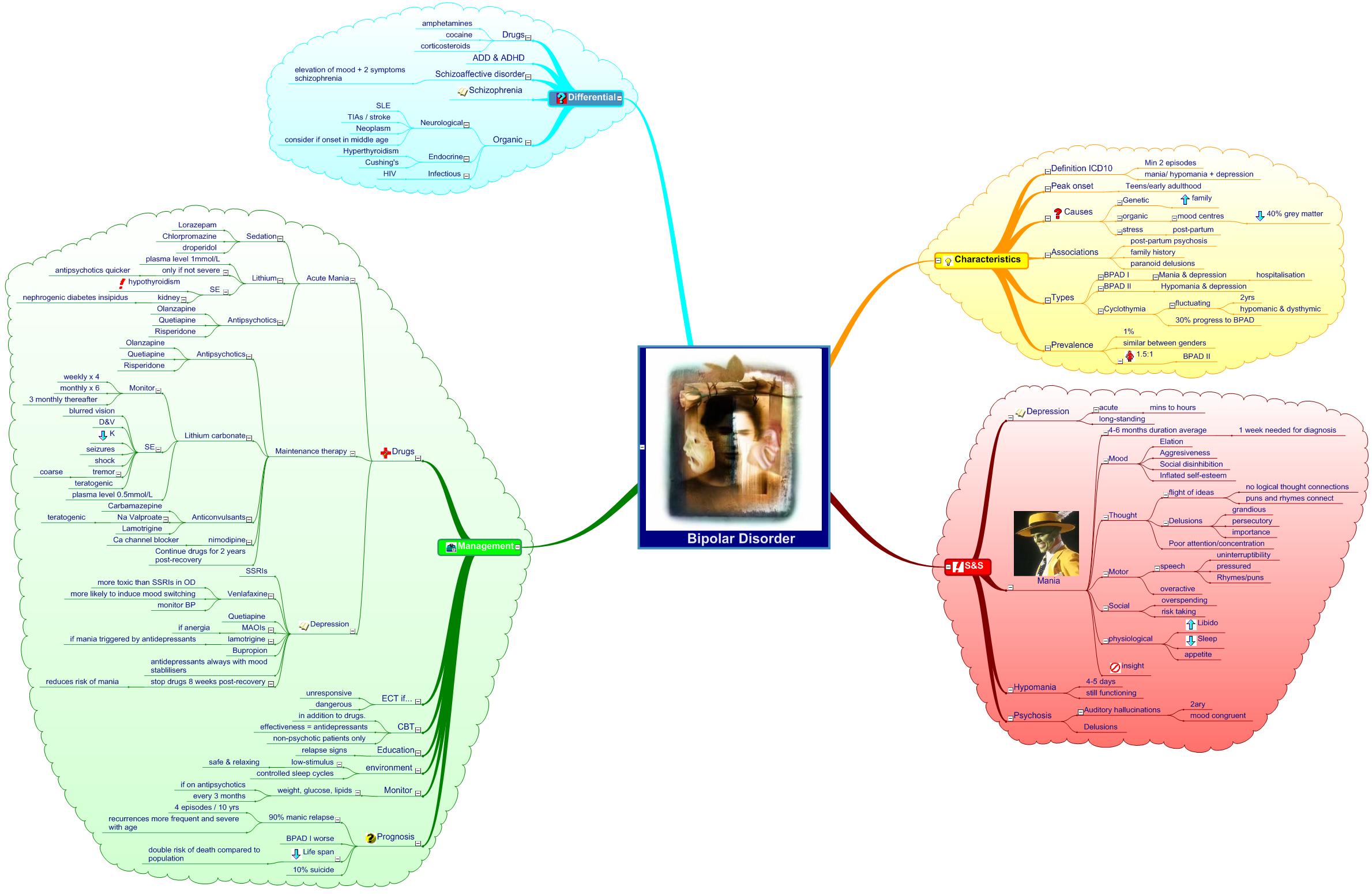
Bipolar Disorder |
please flag with care:
| |
| 2007-12-24 | No history |  | Add My version | |
| Download temporary blocked | | |
| Mind map Bipolar Disorder (from MedMaps.co.uk) - the online mind map resource for medical students and doctors. Psychiatry. Medicine. | |
 | |
| outline | |
Bipolar Disorder
Characteristics
Definition ICD10
Min 2 episodes
mania/ hypomania + depression
Peak onset
Teens/early adulthood
Causes
Genetic
family
organic
mood centres
40% grey matter
stress
post-partum
Associations
post-partum psychosis
family history
paranoid delusions
Types
BPAD I
Mania & depression
hospitalisation
BPAD II
Hypomania & depression
Cyclothymia
fluctuating
2yrs
hypomanic & dysthymic
30% progress to BPAD
Prevalence
1%
similar between genders
1.5:1
BPAD II
S&S
Depression
acute
mins to hours
long-standing
Mania
4-6 months duration average
1 week needed for diagnosis
Mood
Elation
Aggresiveness
Social disinhibition
Inflated self-esteem
Thought
flight of ideas
no logical thought connections
puns and rhymes connect
Delusions
grandious
persecutory
importance
Poor attention/concentration
Motor
speech
uninterruptibility
pressured
Rhymes/puns
overactive
Social
overspending
risk taking
physiological
Libido
Sleep
appetite
insight
Hypomania
4-5 days
still functioning
Psychosis
Auditory hallucinations
2ary
mood congruent
Delusions
Management
Drugs
Acute Mania
Sedation
Lorazepam
Chlorpromazine
droperidol
Lithium
plasma level 1mmol/L
only if not severe
antipsychotics quicker
SE
hypothyroidism
kidney
nephrogenic diabetes insipidus
Antipsychotics
Olanzapine
Quetiapine
Risperidone
Maintenance therapy
Antipsychotics
Olanzapine
Quetiapine
Risperidone
Lithium carbonate
Monitor
weekly x 4
monthly x 6
3 monthly thereafter
SE
blurred vision
D&V
K
seizures
shock
tremor
coarse
teratogenic
plasma level 0.5mmol/L
Anticonvulsants
Carbamazepine
Na Valproate
teratogenic
Lamotrigine
nimodipine
Ca channel blocker
Continue drugs for 2 years post-recovery
Depression
SSRIs
Venlafaxine
more toxic than SSRIs in OD
more likely to induce mood switching
monitor BP
Quetiapine
MAOIs
if anergia
lamotrigine
if mania triggered by antidepressants
Bupropion
antidepressants always with mood stablilisers
stop drugs 8 weeks post-recovery
reduces risk of mania
ECT if...
unresponsive
dangerous
CBT
in addition to drugs.
effectiveness = antidepressants
non-psychotic patients only
Education
relapse signs
environment
low-stimulus
safe & relaxing
controlled sleep cycles
Monitor
weight, glucose, lipids
if on antipsychotics
every 3 months
Prognosis
90% manic relapse
4 episodes / 10 yrs
recurrences more frequent and severe with age
BPAD I worse
Life span
double risk of death compared to population
10% suicide
Differential
Drugs
amphetamines
cocaine
corticosteroids
ADD & ADHD
Schizoaffective disorder
elevation of mood + 2 symptoms schizophrenia
Schizophrenia
Organic
Neurological
SLE
TIAs / stroke
Neoplasm
consider if onset in middle age
Endocrine
Hyperthyroidism
Cushing's
Infectious
HIV
|
| |